By Jia H. Jung, California Local News Fellow
When Jocelyn “Josie” Howard visited South Dakota from Hawai’i, she stopped at a Walmart in the tiny city of Huron and immediately saw people of Micronesian heritage like herself. They turned out to be her nephew and his wife. When their phone rang, it was the hospital calling with information about their prematurely born baby. The person on the other end of the line asked whether they had an interpreter nearby.
The couple, not confident in English, looked to Howard. The Micronesian co-founder and CEO of Honolulu-based non-profit We Are Oceania stepped in to help – something she was used to doing in her daily work to ensure that Micronesians and Pacific Islanders can be self-sufficient in Hawai’i and on the mainland.
Howard shared this anecdote on Tuesday in a webinar hosted by the White House Initiative on Asian Americans, Native Hawaiians, and Pacific Islanders (WHIAANHPI) and Centers for Medicare & Medicaid Services (CMS). She said that she returned to Hawai’i with a heavy heart, knowing that there are so many others who receive poor or no health care because of language barriers and a lack of assistance navigating systems.
“Some of these hospitals are denying procedures because the patient does not understand what they are about to receive,” she said.

President Joe Biden established WHIAANHPI on May 28, 2021 with Executive Order 14031 to advance equity, justice, and opportunity for Asian Americans, Native Hawaiians, and Pacific Islanders.
The task force tackled the health dimension of this endeavor with its online session encouraging Asian Americans, Native Hawaiians, and Pacific Islanders to sign up for marketplace medical insurance coverage by Dec.15 for coverage beginning on Jan. 1, 2024.
The briefing was CMS’s 11th themed “week of action” since early Oct. 22 targeting specific populations such as Black Americans, veterans, rural residents, gig workers, and American Indians, Alaska Natives, and tribal members. CMS has approached each group with public service announcement materials meant to demystify how to get insurance under the Affordable Care Act signed into law in 2010.
Subsidies from the American Rescue Plan for the COVID-19 crisis mean that the insurance will be cheap – $10 a month for 4 out of 5 people and completely free for some enrollees. An estimator tool at the U.S. government’s healthcare site helps people preview and compare the prices for plans for which they are eligible.
Erika Ninoyu, WHIAANHPI senior advisor and Krystal Ka’ai, executive director of WHIAANHPI and an appointed member of the Presidents’ advisory commission on Asian Americans, Native Hawaiians, and Pacific Islanders, opened up the presentation.

On behalf of the outreach and engagement efforts of 400 CMS officials across 10 regions of the U.S., the WHIAANHPI representatives encouraged all Asian Americans, Native Hawaiians, and Pacific Islanders to go to healthcare.gov/find-assistance or call (800) 318-2596 to find assistants, agents, and brokers to aid in the registration process.
They then opened the floor to four panelists from CMS and three community leaders including Howard for their perspectives on challenges and best practices in sharing healthcare information to people under the AANHPI ethnic designation.
The call to register for marketplace insurance is directed toward all Americans who have never had insurance before, who have to renew their plans, who have turned 26 and aged out of parental coverage, or who are elderly and need to visit a website to access life-saving coverage.
The information also applies to people who have undergone life changes, such as leaving or losing their jobs, purchasing homes, or having a baby.
Others who need to take action are some 15 million people nationwide who will lose eligibility for Medicaid or age out of the Children’s Health Insurance Program (CHIP) coverage in the upcoming year. They have more time – until July 2024 – to switch over to marketplace insurance.

Dr. Ellen Montz, deputy administration and director of the CMS Center for Consumer Information and Insurance Oversight, said that 4.6 million people have registered for coverage so far – over a 50% jump in new enrollees.
She vowed that CMS will not rest until every single American has insurance. She also announced $100 million in grant funding for 60 “navigator” organizations across the country to reduce the intimidation and confusion involved in comparing coverage and signing up electronically for the right plans.
Daniel Tsai, deputy Administrator and director of CMS’s Center for Medicaid and CHIP Services, urged everyone to look out for insurance registration renewal requests arriving via snail mail and actually respond to them. He cautioned that ineligibility of parents does not mean ineligibility for their children, and that adults should be aware of this.
The CMS officials beseeched community leaders to assist in the government’s efforts by taking distributing resources hyperlinked into a comprehensive toolkit and a condensed two-sheeter about renewal after expiration of Medicaid and CHIP coverage. The latter offers translated content in Chinese, Hindi, Korean, Tagalog, and Vietnamese, plus Ukrainian.

Dr. Aditi Mallick, acting director of the Office of Minority Health at CMS, expressed determination to reach more uninsured people with culturally and linguistically tailored sources.
She stated that almost 1 out of 10 people in the U.S. has limited English proficiency. For the aggregate AANHPI group, the figure is far higher at 1 out of 3 – an inequity directly associated with less healthcare access and poorer quality of services received.
Mallick said that improving data collection to help guide how best to serve all AANHPI groups is another top priority and the number one project of the CMS Framework for Health Equity. She also told everyone to expect the Office of Management and Budget’s revisions to 1997 standards for data collection to be completed by next summer.
She said that the bundling of aggregated national health data for AANHPI people masks variations among the groups. For example, the Department of Health and Human Services (HHS) finds that 2.8% of Japanese people are uninsured, in contrast with 12% of Native Hawaiians.

Mallick stated that the president’s budget has incorporated recommendations from the Equitable Data Working Group to increase sample size by surveying more people from smaller demographics. The hope is that “oversampling” will reveal the disparities among AANHPI groups and provide better insight into how to level them.
Stefanie Costello from the CMS communications office asked organizations serving AANHPI communities to direct everyone to Medicare and CHIP Renewals resources online and the Coverage to Care (C2C) website delivering health insurance literacy for first timers like immigrants, aged-out young adults, and the previously uninsured.
The first site features content in Chinese, Hindi, Korean, Tagalog, and Vietnamese – the second has Chinese, Korean, Ukrainian, and Vietnamese materials, though nothing in Hindi or Tagalog. Additionally, Medicare & You, a 128-page booklet, is available in Chinese, Korean, and Vietnamese.
Liza Merrill of Arizona-based Asian Pacific Community in Action (APCA) emphasized a need for health information in even more languages for non-English speakers in AANHPI groups, which are collectively the fastest growing demographic on the North American continent.

And she said that this information must be delivered by people of the community who have built up relationships of trust. “We have to get buy-in in order for them to come into our offices,” she said, of the people CMS is trying to reach.
Lao, Marshallese, and Vietnamese-Chinese health navigators on APCA’s staff provide interpretation of information while logging demographics, family health information, and other notes about their clients into a system storing the valuable in-house data.
“It is not a one and done,” Merrill declared. “Once we enroll them, we become friends.”
In closing, she shared the AA & NH/PI Health Central mega-directory made possible by The NYU Center for the Study of Asian American Health (CSAAH), a National Institutes of Health (NIH) National Institute on Minority Health and Health Disparities (NIMHD)‒funded Specialized Center of Excellence.
The database centralizes organizations across the country, searchable by AANHPI subgroup and focus, including areas like arts and culture and professional development as well as health education and social services.

Howard, who shared her experience with the underserved Micronesian community in middle America, reiterated the need for trusted community members who speak key languages and have the cultural understanding to make healthcare seekers comfortable.
She also talked about the differences in cultural fluency and digital literacy across states. She said that Hawai’i has substantial unhoused and employed populations struggling to get by in one of the most expensive places to live in the country.
Yet, Hawai’i is capable of taking fast action in getting people health coverage during times of crisis because of its long journey in obtaining and maintain Medicaid access for its most vulnerable community members such as the poor and aging.
One fight in Hawai’i to protect the health justice for underserved Micronesians began in 1996, when Congress passed the Personal Responsibility and Work Opportunity Reconciliation Act. The broad welfare reform took away health benefits from people originating from Compact of Free Association (COFA) countries.
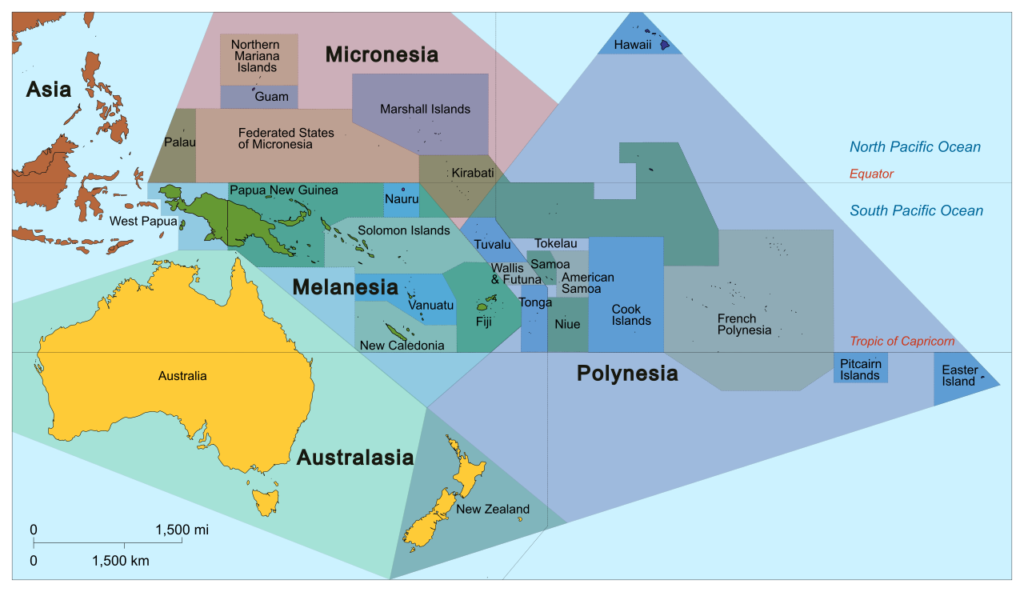
COFA nations emerged out of U.S. “trust territories” established across Micronesia by a U.N. mandate in 1947 in the wake of World War II. The U.S. did not sufficiently protect the territories or build up their infrastructure. Instead, it created more economic and public health challenges, such as by testing the majority of its nuclear weapons offshore the Marshall Islands from 1946 through 1958.
In the 1980s, in a bid to do better, the U.S. formed special COFA relationships with the Republic of Palau, the Republic of the Marshall Islands (RMI), and Yap, Chuuk, Pohnpei, and Kosrae, which make up the Federated States of Micronesia (FSM). People began to flow out of the COFA islands toward labor opportunities in the U.S.. Lately, climate change refugeeism has become a major driver of the Micronesian exodus to the U.S., as rising sea levels put more of the low-lying Micronesian (Greek for “tiny island”) region under water.
When people from these countries lost healthcare in the 1990s, the State of Hawai’i picked up the burden of offering coverage until 2010, when budget strains prompted a challenge to the federal government. The U.S. restored healthcare for people from COFA nations in December 2010 under enforcement of the 14th constitutional amendment of 1868, which promised “equal protection” of American laws to born and naturalized U.S. citizens.
In the past year, We Are Oceania expanded to mainland states such as Iowa, South Dakota, North Carolina, and Tennessee, where Micronesian and Pacific Islanders have far less access to services than they do in Hawai’i.
Nhien Le of the national health advocacy organization Asian Pacific Islander American Health Forum (APIAHF) reinforced the priorities shared by Merrill and Howard. He said that APIAHF tries to affect the big picture by advocating for federal funding for linguistically and culturally appropriate healthcare navigation and policy changes promoting data disaggregation for AANHPI groups.

APIAHF also activates networks of local organizations to create translated materials fine-tuned by community review to relay critical health information. Le said that local organizations helped render updates about the bivalent COVID-19 vaccine into 36 different AANHPI languages.
Audience questions toward the end of the hour ranged from the specific – whether Cantonese and Shanghainese materials would ever be provided – to the broad.
An attendee of the briefing asked how millennials can help elders 65 years and older. Perrie Briskin, a senior advisor at Medicare, said that millennials would do well to first help themselves and their own fellow millennials, as healthy, younger people tend to lag in addressing insurance matters.
Mallick responded that AANHPI millennials can lend digital literacy to help their elders enroll and then follow up with by helping them actually using their healthcare.
She said that “just having someone by your side, whether that’s family or chosen family” is important.
AsAmNews is published by the non-profit, Asian American Media Inc.
We’re now on BlueSky. You can now keep up with the latest AAPI news there and on Instagram, TikTok, Facebook, YouTube and X.
We are supported by generous donations from our readers and by such charitable foundations as the Robert Wood Johnson Foundation.
You can make your tax-deductible donations here via credit card, debit card, Apple Pay, Google Pay, PayPal and Venmo. Stock donations and donations via DAFs are also welcomed.